30-Day IBS Diet Plan Balancing Bowel Blueprint Is Irritable. To address the challenges of Bowel syndrome. Full meal plan for 30 days. Symptoms of IBS like bloating and pain are eased by the program.
Offers an organized way to deal with irregular bowel movements. It has things in it like cereal, bacteria, and water. The plan is meant to make the gut healthier and ease pain.
There are healthy meals and snacks planned for each day of the plan. Foods that are low in FODMAPs are good for you. Some people make IBS conditions worse. The plan also includes ways to control your food and deal with worry. Focus on being aware of how your culture fits together. Can be bad for your gut health.
When you use the Balancing Bowel Blueprint for Digestive Care. People who have IBS don’t have any symptoms. You can begin the process of making your life better. For 30 days, follow this planned method.
can learn more about the unique food causes of each participant. You can feel better if you start eating in a healthy way. more confident and at ease with handling the problem. For more information visit the website The Diet and Weight Loos.
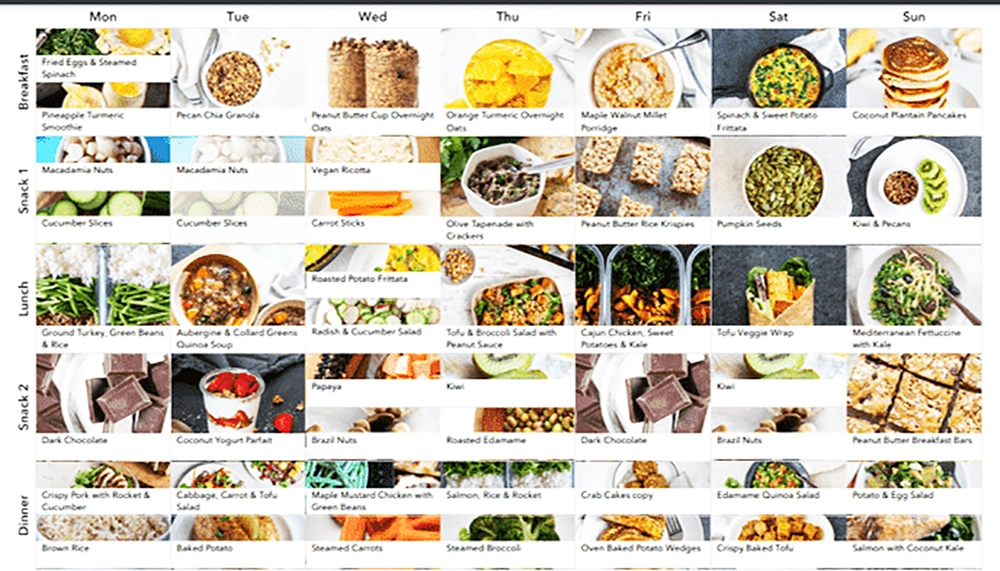
30-day IBS diet plan
30-day IBS diet plan week 1 with individual IBS diet plan. To explain the path to better gut health and help people find their way along it. focuses on teaching important things.
Week 1: Elimination Phase
During the first week, you should focus on cutting out popular foods that make IBS symptoms worse.
- For lunch, I had grilled chicken salad with cucumbers, mixed veggies, and an olive oil sauce.
- Salmon baked in a pan with rice and steamed carrots for dinner.
- As a snack, I like plain yoghurt with nuts and rice cakes with almond butter.
On the first day, people who are taking part get an outline of the IBS eating plan. able to help manage. About how important food is for dealing with IBS. How to get rid of symptoms by following a set plan.
Find out how you can make your life better. Days 2 through 7 A deep understanding of what causes IBS and its symptoms. The subjects’ conditions may get worse because of the results.
gives it useful information. Avoid popular foods that set off your symptoms. understands the link between what they eat and how often their symptoms show up. Participants are also important to the meal plan.
Some topics are covered, such as part control. An important part of handling IBS is making sure you get enough to eat at each meal. Get useful tips for food shopping as well.
Find out how to read food labels and choose the right goods. Must be able to confidently move through the grocery store lanes. At the end of the first week, people know the basics about IBS. For good digestion with a plan for IBS. With all the tools they need to begin their trip.
Week 2-3: Reintroduction Phase
Reintroducing possible trigger foods slowly, one at a time, will help you figure out which ones cause the symptoms.
- Every day, slowly add back in one of the following trigger foods:
- Items made from milk (yoghurt, cheese)
- Grains with gluten (like bread and pasta)
- Foods that are high in FODMAPs include apples, onions, broccoli, and fried foods and rich sauces.
- After returning each food, carefully watch for changes in symptoms.
- For the rest of the meals, stick to low-FODMAP choices to keep things in balance.
- In order to keep track of your symptoms and find causes, keep a food log.
During week 2,
A low-FODMAP phase starts for the participants. Different types of IBS diet plans focus on different parts. Limiting fermentable sugars can help ease your symptoms.
On the 8th day,
Low-FODMAP foods are presented to people. Usually better for people with IBS because it’s easy on their gut system. Find out about the types of FODMAPs that can be fermented. Find out how to pick foods that are low in chemicals.
Days 9 to 14 focus on practical implementation
People who took part ate a range of low-FODMAP foods. It gives you meal plans and recipes. The resources follow the low-FODMAP rules. Gives you ideas and instructions for making healthy, tasty meals.
Tastes and nutritional needs of participants. To find the best thing. While the people who took part ate a low-FODMAP diet. Learn useful things about going out to eat.
Tell the diner staff what you need on the menu. In order to confidently choose the right menu items. Learn how to handle yourself in social settings.
By the end of week 2,
Help people with IBS deal with their problems. with recipes and methods they know how to use. Low-FODMAP food has been built on a strong base.
During week 3,
The people who were on the IBS diet plan moved on to the restart phase. Find your own cues and make your own meal plans. bring back foods that contain FODMAPs.
Mostly about the beginning. From the fifteenth day on, players. brings back into the diet certain types of FODMAPs. Glucose, fructose, galactose, and polyols are the different types of sugars. 30-Day IBS Diet Plan to Manage IBS Symptoms. In regaining control over health and happiness. Acts as the foundation for long-term success.
Over 15 to 21 days,
After the players put each FODMAP group back together. It keeps an eye on the signs. Digestive pain, bloating, or other IBS. Keep thorough records to keep track of how your symptoms change over time.
People can figure out which FODMAPs are making their symptoms worse through this process. Can add something that can be accepted. Participants plan meals based on what they see.
By changing, adding, or taking away FODMAPs. cause symptoms, including ones that can be easily dealt with. Procedures are customized to meet the specific food needs and tastes of each person.
It lets you make meal plans. Helps with long-term control of symptoms and quality of life.
At the end of 3 weeks,
The participants learned a lot about their own FODMAP factors. The best foods for relieving symptoms and making your stomach feel better. Know how to continue customizing and have the tools you need to do it.
During week 4,
Customization of the IBS food plan by participants. Where it’s marked, it moves into the care phase. Getting better at making meal plans based on triggers.
Holistic way of life to handle symptoms over time. The goal changes to adding habits.
Make a personalised meal plan based on the return phase that takes into account your specific triggers and limits.
Day 22–30: Plan meals based on the foods that the person could handle during the return phase.
- To keep your gut system healthy, eat a lot of fibre from low-FODMAP foods like spinach, carrots, and rice.
- Drink lots of water, herbal teas, and fruit-infused low-FODMAP water to stay refreshed.
- To keep your gut healthy, eat foods like yoghurt and kefir that are high in probiotics.
- Try eating smaller meals more often to see if that helps you deal with your problems.
- Keep an eye on the signs and make changes to the food as needed.
From 22 days,

Participants agree on their own personal tastes and limits. Meal plans come with meals. Start making changes to it. The lessons learned during the return process are fair.
Used to make healthy foods that are good for your gut system. Participants have IBS symptoms in addition to making changes to their food. In order to deal with the effects of psychological issues.
Look at ways to deal with stress. In order to improve mental health and ease stomach pain. Learn how to relax, be more aware, or use other stress-relieving methods.
Staying hydrated and regular will help keep participants’ gut health in good shape. It emphasizes how important exercise is. Make sure you drink enough water throughout the day and keep your digestive system healthy.
For example, walking or yoga can help your general health. People are urged to do moderate amounts of physical exercise.
By the end of 4 weeks,
personalized meal plans for each participant. used methods for dealing with stress. Putting water and exercise first. Set the stage for long-term control of symptoms and better quality of life.
During week 5,
People start a time of thinking about the past and making plans for the future. Building on success and taking care of IBS issues. Offers ongoing help and methods for success.
On the 29th day,
People take time to think about the trip they’ve been on for 30 days. Celebrates successes and points out places where more growth is needed.
Look at how the signs have grown. Finds lingering problems by focusing on changes.
Some general tips:
Stay hydrated: To help your stomach, drink a lot of water throughout the day.
Mindful eating: To help your stomach and lower your risk of getting sick, eat slowly and chew your food well.
Dealing with stress: Do things to relieve stress, like yoga, meditation, or deep breathing, because worry can make IBS symptoms worse.
Regular exercise: Doing regular physical movement can help your digestive health and ease your problems.
Remember that everyone has different triggers and limits, so it’s important to work closely with a doctor or chef to create a custom IBS diet plan that works for you.
Day 30 is devoted to future planning strategies:
After the 30-day program is over, participants keep up their work. By making plans and making environmentally friendly habits a part of daily life. Some of these are making meals and learning how to deal with stress.
Goals for staying hydrated and workout plans are made to fit each person’s needs. Resources to help members on a regular basis. Getting people to try new things, like joining support groups. Taking part in online groups. Resources give you useful knowledge, support, and a way to be held accountable. Because the subjects are managing their symptoms for a long time. Keeps them on the path to a better quality of life.
Final word,
30-day IBS diet plan to help people manage their symptoms. An outline for making life better. It takes a look at the whole picture. Last on the food list, press the food recognition button.
By paying close attention to how they use stress-reduction techniques. The participants learned a lot about gut health. Learned useful ways to ease their symptoms.
People in the program eat certain things based on their conditions. found the results and came up with the plan. Comfort from pain and swelling.
Water, frequent exercise, and good gut health. Also learned how important it is to reduce stress to help. When the program is over, the trainees’ gut health is better.
With the knowledge and tools to keep going on the path until. Made changes to their living. Found means to provide ongoing help.
With continued commitment to a healthy food and way of life. Participants kept up with managing their symptoms and planning for the next day. You can wait weeks for better health.
FAQ:
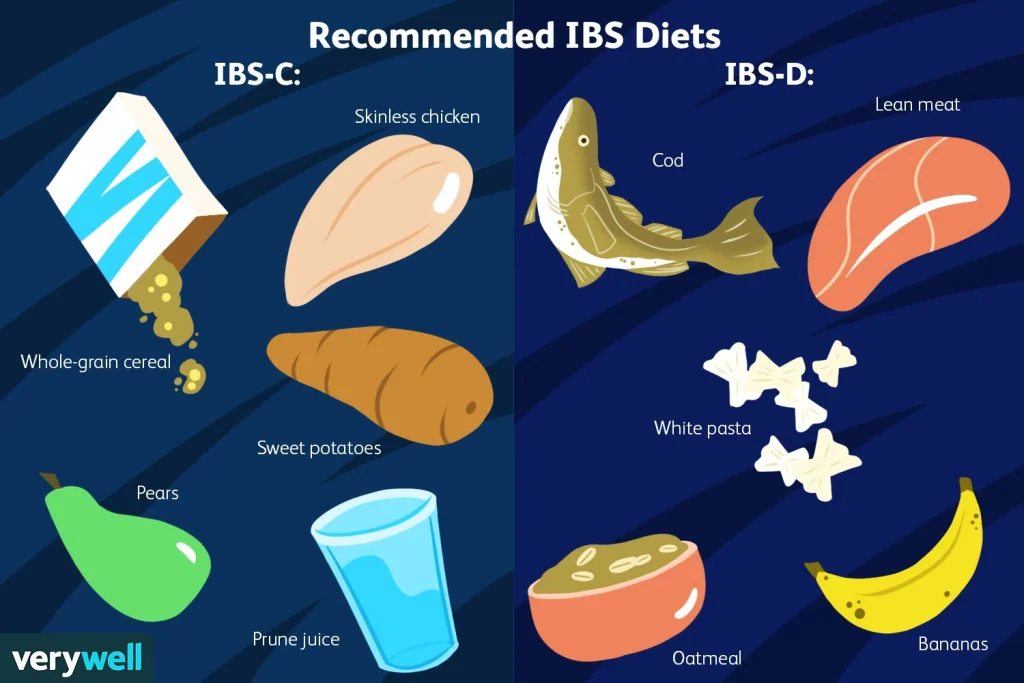
Q: What is the best diet for irritable bowel syndrome?
A: One of the best ways to eat for people with irritable bowel syndrome (IBS). People often stick to a low-FODMAP diet. IBS can make symptoms worse. IBS people can feel better by cutting back on high-FODMAP foods.
Like gas, bloating, stomach pain, diarrhoea, or not being able to go to the bathroom. Get rid of your problems. Get a lot of fiber from foods that are low in FODMAPs. It is good for you to stay hydrated and eat lean protein.
Adding fat is what you need to do. Meal plans that are made just for you. Meets the wants and desires of each person.
Q: What should I eat for breakfast if I have IBS?
A: If you have IBS, choose low-FODMAP foods for breakfast. One food that is made with lactose-free milk is rice. Add some berries or banana slices on top. Or, yoghurt without lactose, veggies, and food that is low in FODMAPs.
Drink smoothies that aren’t too big. You could also have scrambled eggs or tofu with spinach and peppers. Like toast made with gluten-free grain or rice. Pick out a few low-FODMAP foods. Based on what the body tells you and your own capacity. healthcare experts for personalized advice that fits their needs. You should talk to a trained dietitian right away.
Q: What foods help calm IBS?
A: Foods that can help ease the symptoms of IBS. Most of the time, they are easy to stomach and low in FODMAPs. Chicken, turkey, fish, and tofu are all good sources of lean protein.
Fruits that are low in FODMAP include carrots, bananas, grapes, berries, and citrus fruits. Add spinach, bell pepper, zucchini, and cucumber. Pick foods that don’t have gluten, like corn, rice, quinoa, and oats.
Drink a lot of water and eat small meals often. Based on what the body tells you and your own capacity. If you need help making changes to your diet, talk to a medical provider. Talk to a qualified chef.
Q: Is coconut water good for IBS?
A: Some people with IBS may be able to drink coconut water. It has been added and is low in FODMAPs. Keeps you hydrated without adding sugar or fake ingredients.
Tolerances may vary. Some people with IBS may see. Some components of coconut water such as natural sugars or electrolytes. Symptoms can start when you take too much. What happens to the body when you drink a small amount of coconut water? It’s good to pay attention.
Getting advice from a nutritionist can be helpful.